06/09/2024
ByWinner Medical
 37194
37194

Pressure ulcers, also known as bedsores, are localized injuries to the skin and underlying tissue, primarily caused by prolonged pressure on the skin. They are a significant concern in patients with impaired mobility or those confined to bed rest.
Early detection and the use of advanced wound dressings are crucial in improving patient outcomes and preventing severe complications. This article explores the best practices and products for managing pressure ulcers effectively.

Pathophysiology
Pressure ulcers develop due to sustained pressure, which restricts blood flow and leads to ischemia, hypoxia, and tissue necrosis. This condition often occurs over bony prominences, where the pressure is greatest (1). Understanding these pathophysiological mechanisms is essential for preventing and treating pressure ulcers effectively.
Clinical Assessment
Regular clinical assessment is vital for managing pressure ulcers. High-risk patients should undergo frequent skin inspections, and tools like the Braden Scale can help assess risk levels. This scale evaluates factors such as sensory perception, moisture, activity, mobility, nutrition, and friction/shear (2). Early identification allows for timely intervention, reducing the risk of severe complications.
Common Sites and Causes of Pressure Ulcers
Common Sites: Pressure ulcers commonly appear over bony prominences, including the tailbone, buttocks, heels, spine, elbows, ankles, and shoulder blades. They can also develop on the back of the head, shoulders, and ears (1).
Causes:
· Pressure: Prolonged pressure restricts blood flow, leading to tissue damage (1).
· Friction: Friction between the skin and surfaces such as bed sheets or wheelchair mats can damage fragile skin, especially when damp (1).
· Shear Forces: When the body moves in one direction while the skin remains in place, shear forces can damage the skin and underlying tissues (1).
· Moisture: Damp environments, such as those caused by urinary incontinence, can soften the skin and reduce its resistance (1).
Risk Factors
· Decreased Mobility: Patients with limited mobility due to conditions such as paralysis, injury, or surgery are at higher risk of developing pressure ulcers. Inability to change positions frequently leads to prolonged pressure on certain areas of the body, causing tissue damage (2).
· Malnutrition: Adequate nutrition is essential for maintaining skin integrity and supporting the body's natural healing process. Malnourished individuals may experience muscle wasting and loss of protective fat, making the skin more vulnerable to pressure ulcers. Insufficient protein, vitamins, and minerals can also impair the body's ability to repair damaged tissues (2).
· Prolonged Exposure to Moisture: Prolonged exposure to moisture from sweat, urine, or feces can soften the skin, increasing its susceptibility to damage. Conditions such as urinary or fecal incontinence exacerbate this risk by keeping the skin constantly damp, increasing the likelihood of skin breakdown and other complications. (1).
· Anemia and Endothelial Dysfunction: Anemia reduces the oxygen-carrying capacity of the blood, leading to decreased oxygen supply to tissues. Endothelial dysfunction impairs blood flow and vascular health, both of which are crucial for tissue viability and repair. These conditions can slow the healing process and increase the risk of pressure ulcer development (2).
· Lack of Pain Sensation: Patients with conditions that impair sensory perception, such as spinal cord injuries or neuropathy, may not feel pain or discomfort from prolonged pressure. This lack of sensation prevents them from repositioning to relieve pressure, leading to continuous tissue damage and ulcer formation (2).
Grade Treatment of Pressure Ulcers
Grade 1
· Clinical Signs: Redness and swelling without receding, lasting over 30 minutes, with erythema that does not fade.
· Treatment Principle: Protect, clean, and disinfect the skin surface.
· Protective Options: Hydrocolloid dressings and heel foam dressings. Use silicone foam dressings to cushion areas at risk of friction (3).

Grade 2
· Clinical Signs: Partial skin loss with purplish-red skin induration and pain, presenting as pink open wounds or ruptured serum blisters.
· Treatment Principle: Protect wounds from friction, relieve pressure, manage blisters, and control exudate.
· Wound Protectors: Skin protective barriers or foam dressings.
· Exudate Control: Hydrocolloid dressings and foam dressings for mild to moderate exudates (3).

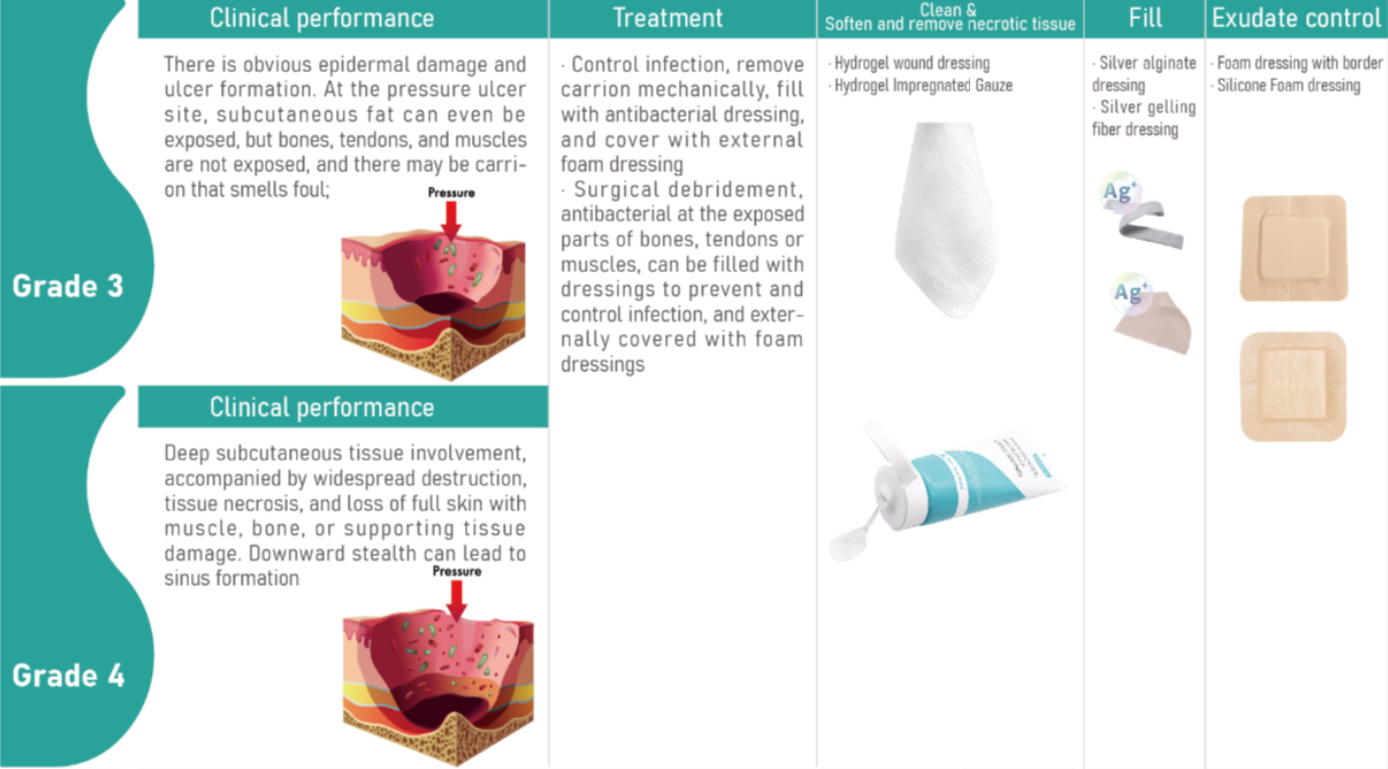
Grade 3
· Clinical Signs: Obvious epidermal damage exposing the subcutaneous fat layer, with foul-smelling carrion.
· Treatment Principle: Debride carrion mechanically, fill wounds appropriate dressings, and cover with foam dressings.
· Remove Necrotic Tissue: Hydrogel dressings and hydrogel impregnated gauze to clean and soften wounds.
· Fill the Wound: Use silver alginate dressings and silver gelling fiber dressings to to help maintain a clean wound environment.
· Exudate Control: Foam dressings with borders and silicone foam dressings to maintain moisture balance (3).
Grade 4
· Clinical Signs: Full-thickness tissue loss exposing muscle and bone, with possible sinus formation.
· Treatment Principle: Surgical debridement, appropriate wound management, filling, and covering the wound with dressings.
· Treatment Methods: Similar to grade 3, using advanced dressings under medical guidance (3).
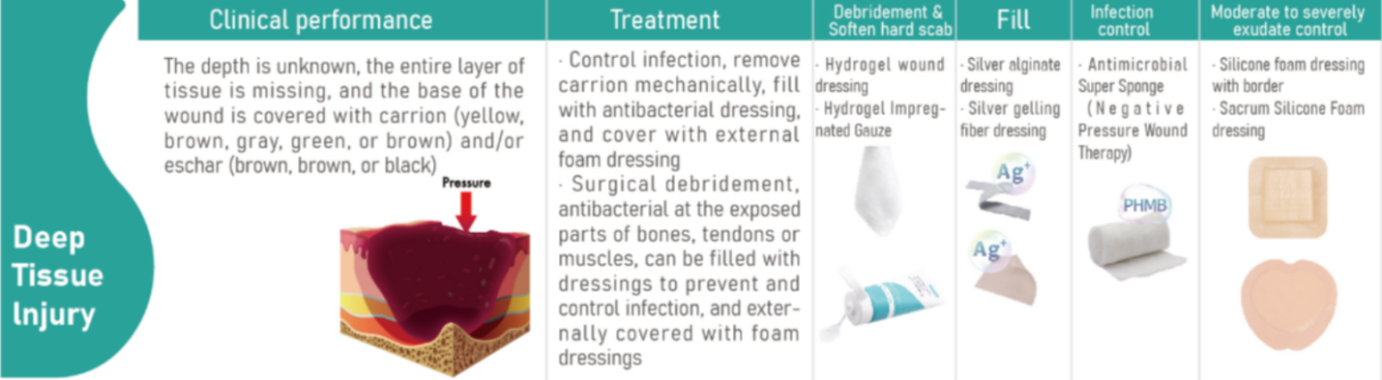
Deep Tissue Injury
· Clinical Signs: Unknown wound depth, possibly covered with carrion or eschar.
· Treatment Principle: Manage the wound environment, remove carrion, and fill the wound with dressings.
· Dressings: Hydrogel dressings to soften scabs, silver alginate dressings for filling, appropriate dressings to maintain a clean wound environment, and silicone foam dressings for exudate management (3).
Preventing Pressure Ulcers
Preventing pressure ulcers requires a multifaceted approach involving regular patient assessments, skin care, proper nutrition, and the use of appropriate support surfaces. Here are detailed strategies for prevention:
1. Regularly Adjust Posture
Patients who are bedridden or sitting for long periods should have their positions changed frequently to redistribute pressure and reduce the risk of ulcer formation. For bedridden patients, turning every two hours is recommended, while those in wheelchairs should shift their weight every 15 minutes. Specialized mattresses and cushions can also help alleviate pressure on vulnerable areas (1).
2. Skin Care
Maintaining healthy skin is crucial in preventing pressure ulcers. The skin should be kept clean and dry to prevent breakdown. Use gentle cleansers and avoid hot water, which can dry out the skin. Moisturize regularly to maintain skin elasticity. Incontinence products that wick moisture away from the skin can also be beneficial. Inspect the skin daily for early signs of pressure damage, such as redness or blisters (1).
3. Nutrition and Hydration
Adequate nutrition and hydration are essential for skin health and healing. Ensure patients receive a balanced diet rich in protein, vitamins (especially vitamins A and C), and minerals (such as zinc) that support tissue repair. Hydration is equally important; encourage patients to drink sufficient fluids to keep the skin hydrated and resilient (2).
4. Support Surfaces
Use pressure-redistributing mattresses, cushions, and overlays to minimize pressure on vulnerable areas. These support surfaces are designed to distribute weight more evenly and reduce the risk of pressure ulcer development. Foam, gel, and air-filled devices can be particularly effective in preventing pressure points (1).
5. Patient and Caregiver Education
Educate patients and caregivers on the importance of repositioning, skin care, and nutrition. Teach them how to recognize early signs of pressure ulcers and the steps to take if they notice any changes. Empowering patients and caregivers with knowledge can significantly reduce the incidence of pressure ulcers (2).

How Winner Medical Helps in Managing Pressure Ulcers?
Pressure ulcers require timely and appropriate treatment tailored to the severity and characteristics of the wound. Advanced wound dressings play a critical role in protecting wound sites, absorbing exudate.
Winner Medical is committed to providing high-quality, effective wound care solutions that support healthcare providers and improve patient outcomes. Our extensive range of products, backed by dedicated research and development, ensures that patients receive the best care across all stages of pressure ulcer management.
By leveraging innovative materials and advanced technologies, Winner Medical’s products support the body's natural healing process while enhancing patient comfort and safety. Whether you are looking for dressings to manage mild skin irritation or severe deep tissue injuries, Winner Medical offers a comprehensive selection to meet diverse clinical needs.
Our ulcer wound dressing products include (but are not limited to):
· Hydrocolloid Dressings: Ideal for Grade 1 and 2 ulcers, these dressings maintain a moist wound environment, protecting the wound from external contaminants (3).
· Hydrogel Dressings: Used in Grades 3 and 4 ulcers, hydrogel dressings help debride necrotic tissue and maintain a moist wound environment, which is essential for healing (3).
· Heel Foam Dressings: Specially designed for the heel area, these dressings provide excellent cushioning and protection against friction and pressure (3).
· Silicone Foam Dressings: These are suitable for all grades of pressure ulcers, especially effective in cushioning bony prominences and managing exudate while minimizing pain during dressing changes (3).
· Silver Alginate Dressings: These dressings are infused with silver ions, designed to help maintain a clean wound environment in deep wounds and ulcers. (3).
· Silver Gelling Fiber Dressings: These are used for filling deep wounds, providing moisture balance and helping to maintain a clean wound environment. (3).
· Sacrum Silicone Foam Dressings: Designed for use on the sacrum, these dressings are shaped to fit the area perfectly, providing protection and absorption of exudate (3).
For more information on our wound care range and how our solutions can benefit your patients, please contact us. Trust Winner Medical to be your partner in delivering superior wound care and improving the quality of life for those at risk of or suffering from pressure ulcers.
Frequently Asked Questions (FAQ) About Wound Dressings for Pressure Ulcers
1. What are pressure ulcers?
Pressure ulcers, also known as bedsores, are localized injuries to the skin and underlying tissue caused by prolonged pressure. They commonly occur in individuals with limited mobility.
2. What causes pressure ulcers?
Pressure ulcers are primarily caused by prolonged pressure on the skin, friction, shear forces, and prolonged exposure to moisture. These factors restrict blood flow and lead to tissue damage.
3. Who is at risk of developing pressure ulcers?
Individuals with decreased mobility, such as those who are bedridden or use a wheelchair, malnourished individuals, those with prolonged exposure to moisture, anemia, endothelial dysfunction, or lack of pain sensation are at higher risk of developing pressure ulcers.
4. How can pressure ulcers be prevented?
Preventing pressure ulcers involves regular repositioning, maintaining skin hygiene, ensuring proper nutrition and hydration, using pressure-redistributing support surfaces, and educating patients and caregivers on early signs and preventive measures.
5. What are the different grades of pressure ulcers?
Pressure ulcers are categorized into four grades:
· Grade 1: Redness and swelling without receding, with erythema that does not fade.
· Grade 2: Partial skin loss with purplish-red skin induration and pain, presenting as pink open wounds or ruptured serum blisters.
· Grade 3: Obvious epidermal damage exposing the subcutaneous fat layer, with foul-smelling carrion.
· Grade 4: Full-thickness tissue loss exposing muscle and bone, with possible sinus formation.
6. What are the best dressings for Grade 1 pressure ulcers?
For Grade 1 pressure ulcers, hydrocolloid dressings and heel foam dressings are recommended. Silicone foam dressings can also be used to cushion areas at risk of friction (3).
7. What are the best dressings for Grade 2 pressure ulcers?
For Grade 2 pressure ulcers, skin protective barriers or foam dressings are suitable for wound protection. Hydrocolloid dressings and foam dressings are effective for controlling mild to moderate exudates (3).
8. What are the best dressings for Grade 3 pressure ulcers?
Grade 3 pressure ulcers benefit from hydrogel dressings and hydrogel impregnated gauze to clean and soften wounds. maintain a clean wound environment, while foam dressings with borders and silicone foam dressings maintain moisture balance (3).
9. What are the best dressings for Grade 4 pressure ulcers?
Treatment for Grade 4 pressure ulcers includes surgical debridement and appropriate wound management, followed by the use of advanced dressings similar to those for Grade 3 ulcers, under medical guidance (3).
10. How does Winner Medical help in managing pressure ulcers?
Winner Medical provides a range of advanced wound care products designed to address various stages and needs of pressure ulcer management. Our products include hydrocolloid dressings, silicone foam dressings, hydrogel dressings, silver alginate dressings, heel foam dressings, silver gelling fiber dressings, sacrum silicone foam dressings, skin protective barriers, and hydrogel impregnated gauze.
11. What makes Winner Medical’s wound care products unique?
Winner Medical’s wound care products are designed with advanced materials, enhanced moisture control, and improved adhesive technologies to ensure secure and effective wound management. These features support the body's natural healing process, enhance patient comfort, and help maintain a clean wound environment.
12. Where can I find more information about Winner Medical’s wound care products?
For more information on our wound care range and how our solutions can benefit your patients, please contact Winner Medical or visit our website. Trust Winner Medical to be your partner in delivering superior wound care and improving the quality of life for those at risk of or suffering from pressure ulcers.
References
[1] Pressure Ulcer. Available at: https://www.ncbi.nlm.nih.gov/books/NBK553107/ (Accessed: 28 May 2024)
[2] Pressure ulcers: Learn More – Preventing pressure ulcers. Available at: https://www.ncbi.nlm.nih.gov/books/NBK326430/ (Accessed: 28 May 2024)
[3] Clinical Practice Guideline: Prevention and Treatment of Pressure Ulcers/Injuries. Available at: https://internationalguideline.com/2019 (Accessed: 28 May 2024)